by Hermes Solenzol
Everything I described in Ask a Neuroscientist: The physiology of BDSM (Part 1) – How Pain Moves to the Brain forms the so-called ascending pain pathway, which goes from the skin to the cerebral cortex. There, in the cortex, is where the pain becomes conscious, it is felt with its particular emotional charge. But, there are also descending pain control pathways that go down from the brain to the spinal cord. Those are critical to understanding why the pain decreases as a sadomasochistic session progresses.
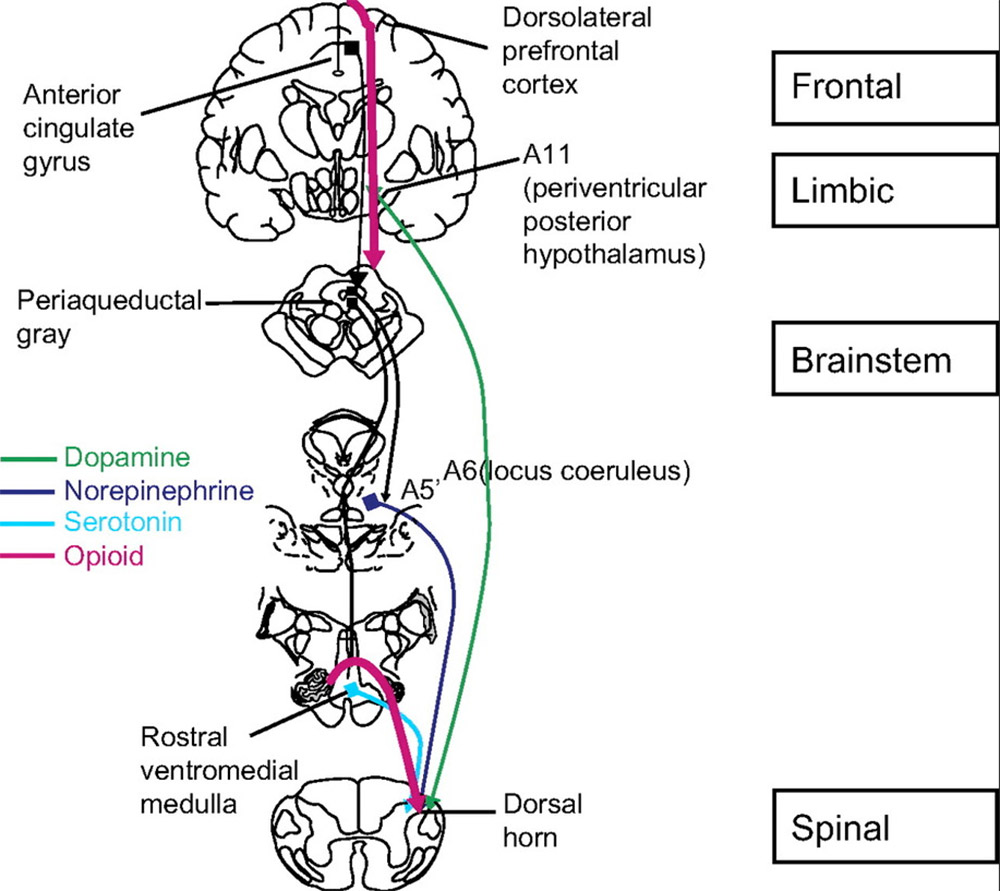
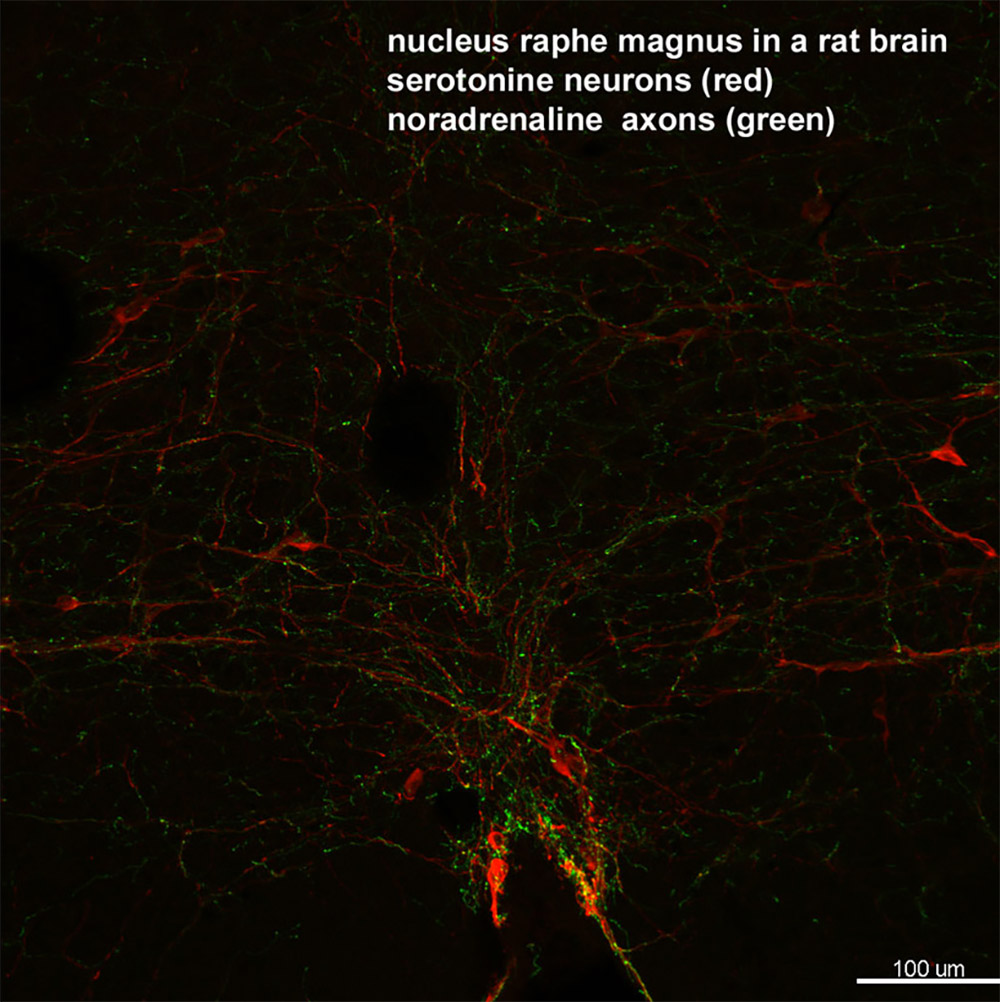
These descending pathways begin in an area in the center of the brain, on the sides of a canal called the aqueduct, which is why it is called a periaqueductal gray (commonly known as PAG). PAG neurons send signals to an area of the medulla, the nucleus raphe magnum, which in turn sends axons down the sides of the spinal cord. These descending nerve fibers penetrate the dorsal horn, which is the area of arrival of nerves coming from the skin. The signals that these descending fibers send from the brain inform the neurons of the dorsal horn of whether they should increase or decrease the pain. Whether they do this in one direction or another depends on our mental state, the emotions generated in the insula and the anterior cingulate cortex.
Everybody knows that a submissive can endure a lot of pain in a scene if the dominant is able to induce a particular mental state in which there is a lot of endorphins release. We imagine that endorphins are like drugs that run through the blood and bathe the whole brain, inhibiting the pain. However, unlike morphine and other opioid drugs, endorphins are not able to cross from blood to the brain. Instead, they are released by neurons in certain areas of the nervous system. One of these areas is the dorsal horn of the spinal cord, where endorphin release is controlled by a particular descending pathway.
However, what are popularly known as “endorphins” (their correct name is “opioids”) are actually a collection of almost 40 different neuropeptides, which are grouped into three families: the endorphins are correctly called the enkephalins and the dynorphins. These neuropeptides act as the keys that activate three types of opiate receptors, named with the Greek letters mu, delta and kappa. The small enkephalins are much more abundant in the nervous system than endorphins and, like them, act on mu and delta receptors to inhibit pain and produce feelings of calm and euphoria. Dynorphins bind to kappa receptors and also decrease pain, but instead of producing euphoria they produce the opposite: dysphoria, which is a very unpleasant state of mind.
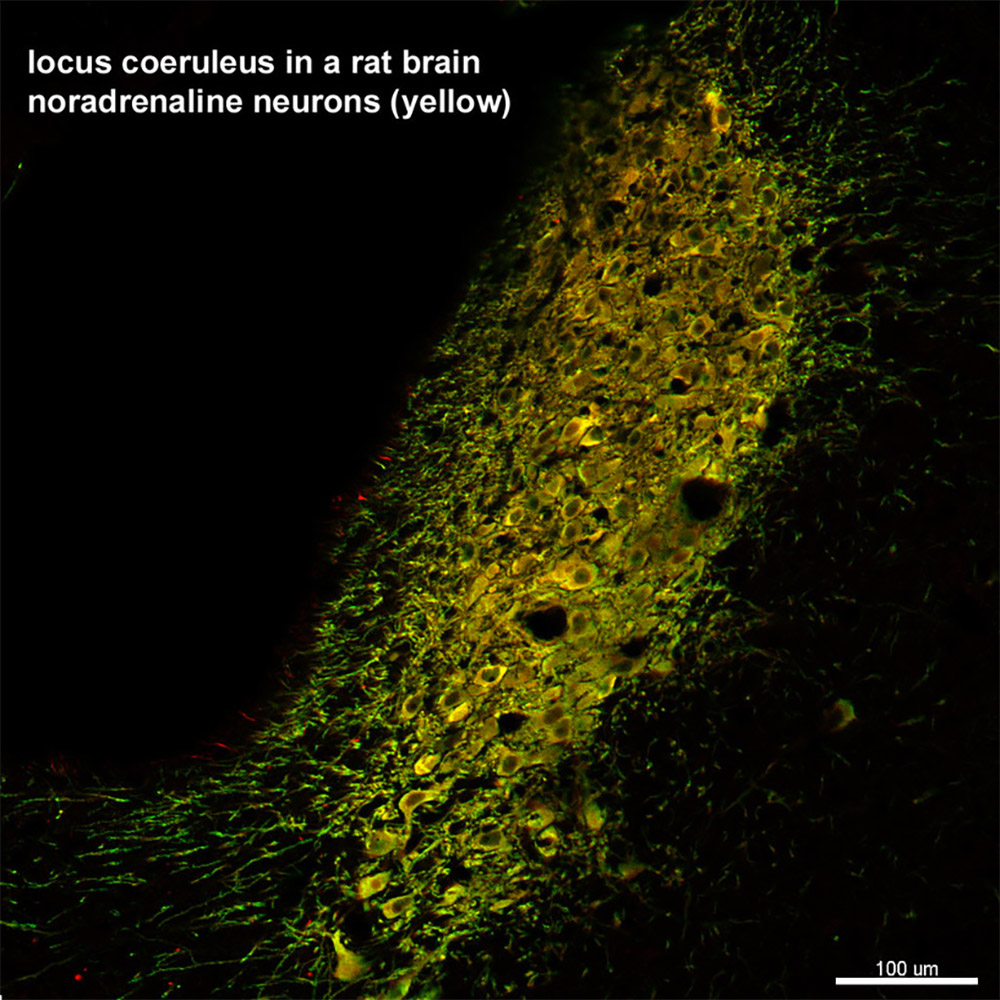
Descending pathways not only inhibit pain using endorphins. Another descending pathway is the noradrenergic pathway, which uses a neurotransmitter called noradrenaline, similar to the hormone adrenaline. The opioid pathway and the adrenergic pathway are not usually active at the same time, but alternate by inhibiting pain in different mental states. The adrenergic pathway is activated in “fight or flight” situations, where we have to respond to something that threatens us with intense muscular activity, either by fighting or by running away. The endorphin pathway, on the other hand, is activated when fear produces a diametrically opposed behavior: instead of fighting or fleeing, we become paralyzed and cannot move, a response called “freezing”. In many animals, this immobility serves to camouflage and not be seen by a predator.
HOW THE SCIENCE WORKS IN BDSM
 How does all this apply to a SM scene? The threatening attitude of the dominant and the first painful sensations probably activate the noradrenergic pathway, producing an “adrenaline rush” that is characterized by the feeling of being more alert and the desire to struggle and complain. However, as the scene progresses the submissive may find him/herself immobilized in bondage and the pain administered continuously and unavoidably. This causes the noradrenergic pathway to be replaced by the endorphin pathway.
How does all this apply to a SM scene? The threatening attitude of the dominant and the first painful sensations probably activate the noradrenergic pathway, producing an “adrenaline rush” that is characterized by the feeling of being more alert and the desire to struggle and complain. However, as the scene progresses the submissive may find him/herself immobilized in bondage and the pain administered continuously and unavoidably. This causes the noradrenergic pathway to be replaced by the endorphin pathway.
Inhibition of pain is now accompanied by a state of relaxation and surrender. The submissive is wrapped in a feeling of calm euphoria. Surely she will not want to abandon that state of well-being, and with her passivity and moans of pleasure she will encourage the dominant to continue administering the pain that keeps her there. She is in what is called “the forever place”, a state she would be reluctant to leave.
There are other descending pathways that use two other neurotransmitters: serotonin and dopamine. However, both of them can either increase or decrease pain by acting on different neurotransmitter receptors in the spinal cord. The serotonergic pathway starts in the raphe nuclei of the medulla, the same place where the endorphin pathways starts.
It is still not very clear what states makes serotonin increase or decrease pain, but they could be related with the sleep-wake cycle – we tend to feel less pain when we are asleep.
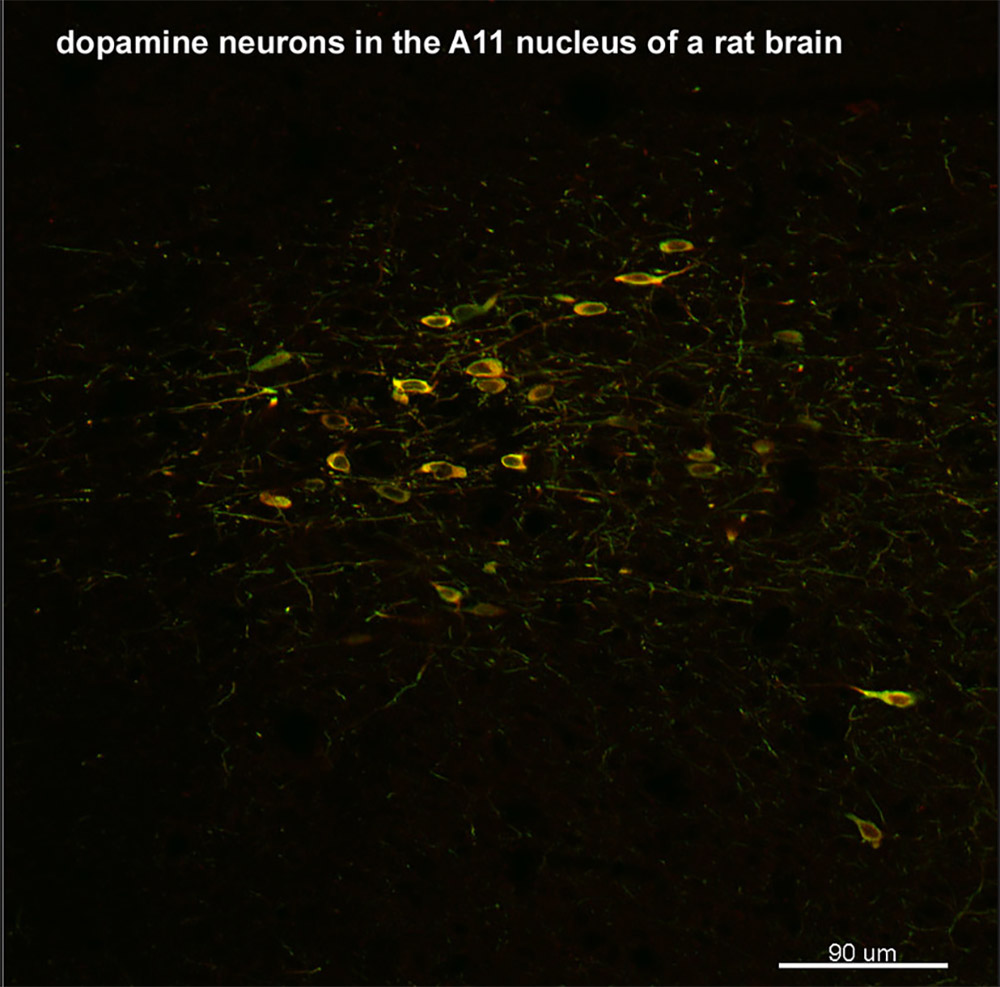
The dopaminergic pathway starts in a nucleus called the A11, located in the middle of the brain on top of the hypothalamus. In the spinal dorsal horn, dopamine can act on D2 receptors and inhibit pain, or on D1/D5 receptors to increase pain. It seems that during chronic pain the D2 receptors become less active and the D1/D5 receptors become more active, so dopamine maintains the state of high pain sensitivity.
How serotonin and dopamine in the spinal cord contribute to the mental states during a scene is anybody’s guess. However, in the brain dopamine acts on the so called “reward pathway” to increase euphoria and positive reinforcement.
FURTHER READING
• Deviance & Desire – Ask a Neuroscientist: Altered States of Consciousness in BDSM
• Deviance & Desire – Endorphins and Adrenaline – What Science Really Says
• Deviance & Desire – Ask a Neuroscientist: Pain Physiology Explained to a Bottom
REFERENCES
- Fields HL, Heinricher MM, Mason P (1991) Neurotransmitters in nociceptive modulatory circuits. Annu Rev Neurosci 14:219-245.
- Gebhart GF (2004) Descending modulation of pain. Neurosci BiobehavRev 27:729-737.
- Hunt SP, Mantyh PW (2001) The molecular dynamics of pain control. Nat Rev Neurosci 2:83-91.
- Jensen TS, Yaksh TL (1984) Spinal monoamine and opiate systems partly mediate the antinociceptive effects produced by glutamate at brainstem sites. Brain Res 321:287-297.
- Le Bars D (2002) The whole body receptive field of dorsal horn multireceptive neurones. Brain Res Rev 40:29-44
- Mason P (1999) Central mechanisms of pain modulation. Curr Opin Neurobiol 9:436-441.
- Sandkuhler J, Gebhart GF (1984) Relative contributions of the nucleus raphe magnus and adjacent medullary reticular formation to the inhibition by stimulation in the periaqueductal gray of a spinal nociceptive reflex in the pentobarbital-anesthetized rat. Brain Res 305:77-87.
- Vanderah TW, Suenaga NM, Ossipov MH, Malan TP, Jr., Lai J, Porreca F (2001) Tonic descending facilitation from the rostral ventromedial medulla mediates opioid-induced abnormal pain and antinociceptive tolerance. J Neurosci 21:279-286.
ABOUT THE AUTHOR
 Based in Los Angeles, California, Hermes Solenzol is a neuroscientist, and has been doing research on pain for several decades. In particular, he has been investigating endorphin release in rats. He has been a sadist for as long as he can remember and active in the scene for several decades.
Based in Los Angeles, California, Hermes Solenzol is a neuroscientist, and has been doing research on pain for several decades. In particular, he has been investigating endorphin release in rats. He has been a sadist for as long as he can remember and active in the scene for several decades.
Much of his writing is published in Spanish at Sexo, ciencia y espíritu, but there’s a great collection of articles on his English site, Sex, science and spirit. Along with a lot of BDSM wisdom, you’ll find thoughts on polyamory, communication, psychology and love.
He’s currently translating his first erotic novel from Spanish to English.

One Comment Add yours